Skin Yeast Infections and Their Link to Allergies - What You Need to Know
 Oct, 20 2025
Oct, 20 2025
Yeast vs Allergy Rash Checker
Symptom Assessment
Answer these questions to identify whether your rash is likely caused by a yeast infection or allergic dermatitis.
Results
Yeast Infection Probability
Allergic Dermatitis Probability
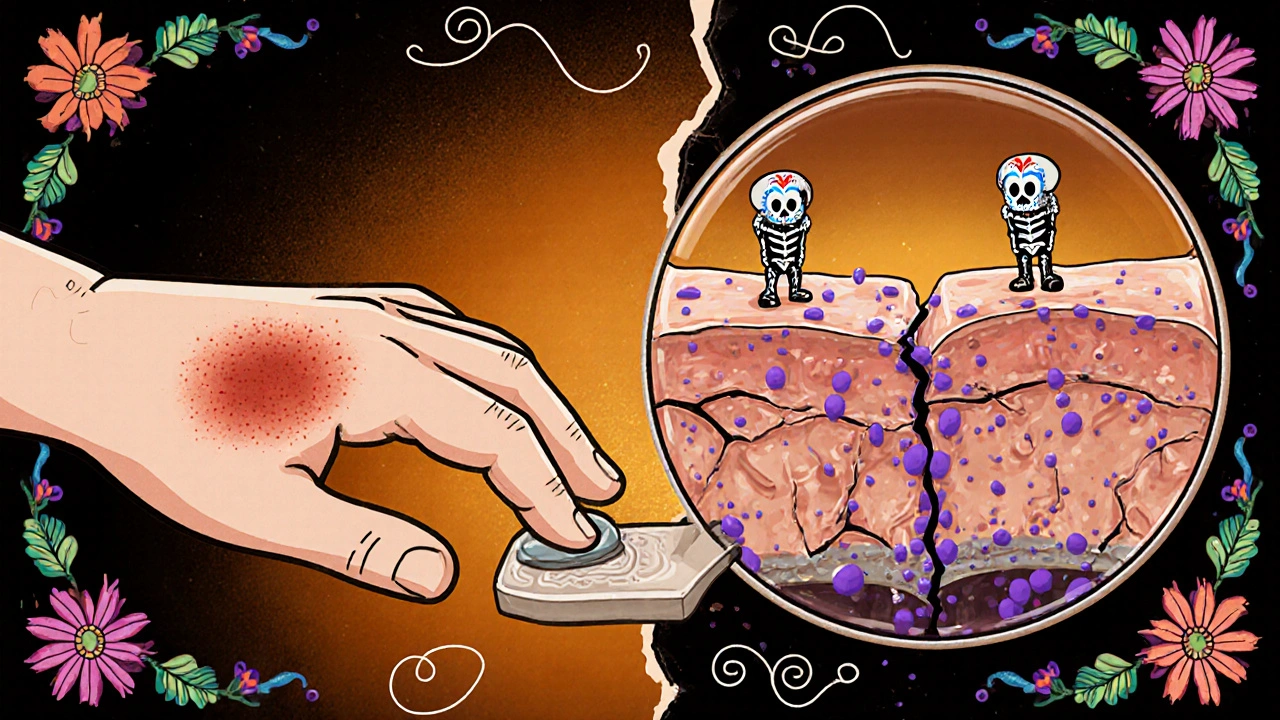
When we talk about yeast infection of the skin, skin yeast infection is a fungal condition that shows up as red, itchy patches, often in warm, moist areas. Many people assume it’s just a hygiene issue, but growing research points to a hidden connection with the body’s allergic responses. In this article you’ll learn why the two often appear together, how to spot the overlap, and what practical steps can break the cycle.
What Exactly Is a Skin Yeast Infection?
Candida albicans is the chief culprit behind cutaneous candidiasis. This yeast lives harmlessly on our skin, mouth, and gut, but when the environment turns warm, humid, or acidic it can overgrow. The overgrowth triggers inflammation, leading to the classic signs: small bumps, scaling, and intense itching.
Typical hot spots include the groin, armpits, under the breasts, and between toes. Anyone can get it, but people with diabetes, obesity, or weakened immune systems are especially prone.
Allergies and the Skin: A Quick Primer
Allergies are immune‑system reactions to substances that the body mistakenly labels as threats. Allergic contact dermatitis occurs when skin touches an allergen like nickel, fragrances, or certain soaps. Atopic dermatitis (eczema) is a chronic, genetically‑linked condition that flares up with allergens, stress, or humidity.
Both types share symptoms-redness, itch, and sometimes blistering-making it easy to confuse them with a fungal infection.
Why Do Yeast Infections and Allergies Often Appear Together?
Three main mechanisms tie them together:
- Immune dysregulation: When the immune system is busy fighting an allergen, it can lose some of its ability to keep yeast in check. The same Th2‑dominant response that drives allergy symptoms also gives yeast an opening to multiply.
- Barrier disruption: Allergic dermatitis damages the skin’s protective barrier, creating a moist, cracked playground for Candida. Conversely, a yeast overgrowth can irritate the barrier, making it more permeable to allergens.
- Microbiome shift: Repeated use of harsh anti‑itch creams or antibacterial soaps to calm an allergic flare can wipe out beneficial bacteria, allowing yeast to dominate the local microbiome.
Understanding this feedback loop is the first step toward breaking it.
Spotting the Overlap: How to Tell If Your Rash Is Yeast, Allergy, or Both
Here’s a quick checklist you can run through at home. If you’re unsure, see a dermatologist.
- Location: Yeast loves warm folds; allergies often hit the wrists, neck, or anywhere the irritant touches.
- Appearance: Yeast usually forms small, uniform pustules with a satiny sheen. Allergic rashes are more likely to be raised, irregular, and may have small vesicles.
- Itch pattern: Yeast itch is steady and worse after sweating. Allergy itch spikes after exposure to the trigger.
- Response to treatment: Antifungal creams improve yeast within days; antihistamines help allergies but do little for a fungal infection.
If you notice mixed signals-e.g., a rash that improves partially with an antifungal but still burns after a day-consider a dual approach.
Managing a Dual Diagnosis: Practical Steps
Below is a step‑by‑step plan that addresses both the fungal and allergic components.
- Confirm the diagnosis: Get a skin scraping or culture from a doctor. Lab results will tell if Candida is present.
- Start an antifungal: Topical clotrimazole 1% cream applied twice daily for two weeks is a common first line.
- Reduce moisture: Keep affected areas dry. Use talc‑free powder and change underwear after sweating.
- Identify and eliminate allergens: Patch‑test or keep a diary of soaps, detergents, and fabrics. Switch to fragrance‑free, hypoallergenic products.
- Apply barrier‑repair creams: Zinc‑oxide or ceramide‑rich moisturizers help restore the skin barrier, limiting both yeast growth and allergen penetration.
- Consider oral antihistamines: If itching persists, a non‑sedating antihistamine like cetirizine can calm the allergic response.
- Probiotic support: Oral probiotic supplements containing Lactobacillus strains may rebalance gut flora, indirectly supporting skin health.
- Re‑evaluate after two weeks: If the rash hasn’t cleared, step up to oral antifungals (e.g., fluconazole) under medical supervision.
Comparison Table: Yeast Infection vs. Allergic Dermatitis
| Feature | Yeast Infection (Candida) | Allergic Dermatitis |
|---|---|---|
| Typical locations | Warm folds (groin, under‑breast, intertriginous zones) | Anywhere the allergen contacts skin (wrists, neck, face) |
| Appearance | Red‑brown patches, satellite pustules, shiny surface | Red, raised, may have vesicles or dry scaling |
| Main trigger | Moisture, high sugar, immune suppression | Nickel, fragrances, latex, foods, pollen |
| First‑line treatment | Topical antifungal (clotrimazole, miconazole) | Remove allergen, topical corticosteroid, antihistamine |
| Diagnostic test | Skin scraping, KOH prep, culture | Patch test or clinical history |

Common Pitfalls and How to Avoid Them
Even with a solid plan, people trip up. Here are the most frequent mistakes and quick fixes.
- Over‑cleansing: Harsh soaps strip the lipid barrier, inviting both yeast and allergens. Stick to gentle, pH‑balanced cleansers.
- Skipping the barrier repair step: Antifungals clear the fungus but leave cracked skin, which can reignite an allergic response. Seal the deal with a ceramide‑rich moisturizer.
- Self‑diagnosing based on pictures: Online images can be misleading. A professional culture can differentiate Candida from a contact dermatitis.
- Ignoring systemic factors: Uncontrolled diabetes or a high‑sugar diet fuels yeast. Manage blood sugar and consider dietary tweaks (reduce refined carbs, increase probiotic foods).
When to Seek Professional Help
If any of the following apply, book an appointment promptly:
- Rash spreads rapidly or covers a large body area.
- You develop fever, chills, or notice pus‑filled lesions.
- Topical treatments give no relief after 5‑7 days.
- You have a chronic condition such as eczema that keeps flaring despite standard care.
Dermatologists can perform a KOH test, prescribe stronger oral antifungals, or recommend phototherapy for stubborn allergic dermatitis.
Bottom Line: Treat Both Sides of the Coin
Yeast infections of the skin and allergies are not isolated problems; they often feed each other. By confirming the diagnosis, cutting moisture, repairing the skin barrier, and removing allergens, you can break the vicious cycle and keep your skin clear.
Can a skin yeast infection cause an allergic reaction?
Yes. When Candida overgrows, it releases metabolites that irritate nerve endings and can sensitize the immune system, making the skin more reactive to allergens.
Is it safe to use antifungal cream and a steroid cream at the same time?
Generally it’s okay for short periods, but you should follow a doctor’s guidance. Steroids can thin the skin and may let yeast spread if used too long.
What home remedies help prevent skin yeast infections?
Keep the area dry, wear breathable cotton, use talc‑free powder, and apply a thin layer of 10% apple cider vinegar diluted with water after washing.
Can diet affect skin yeast infections?
High‑sugar and refined‑carb diets raise blood glucose, creating a favorable environment for Candida. Reducing sugary foods and adding probiotic‑rich yogurt can help.
How long does it take for an antifungal cream to clear a rash?
Most people see improvement within 3‑5 days, but complete clearance often requires a full 2‑week course, even if symptoms fade sooner.
Sebastian Green
October 20, 2025 AT 17:50I totally get how frustrating those itchy spots can be, especially when they pop up in hidden folds. It’s easy to feel embarrassed, but you’re definitely not alone in this. I’ve seen friends struggle with the same cycle of moisture and irritation. The key is to keep the area dry and to use a gentle barrier cream that doesn’t further irritate the skin. Also, try swapping out scented soaps for something fragrance‑free; it can make a world of difference.
Hang in there, and don’t hesitate to get a quick skin scraping if you’re unsure.
Wesley Humble
November 8, 2025 AT 11:30From an analytical standpoint, the pathophysiology described aligns with established immunological models. The Th2‑dominant response indeed compromises antifungal defenses, thereby facilitating Candida proliferation. Moreover, the cited feedback loop between barrier disruption and microbiome shift is substantiated by peer‑reviewed literature. 😊 Nonetheless, adherence to the prescribed regimen remains paramount for clinical resolution.
barnabas jacob
November 27, 2025 AT 06:10Honestly, most people just ignore the underlying immuno‑modulation and keep slappin’ on random creams, which is a classic case of misguided self‑care. The jargon‑heavy reality is that a dysregulated Th2 axis creates a permissive niche for Candida, and the layperson’s “just wash it” approach does nothing but further erode the skin‘s barrier. Also, stop misspelling “antifungal” as “anti fungal” – it’s a single word, bro.
Better to follow evidence‑based protocols than to wing it.
Kirsten Youtsey
December 16, 2025 AT 00:50One must consider the broader sociopolitical matrix that influences dermatological health. The pharmaceutical industry subtly directs our attention toward quick‑fix topical agents while downplaying the role of environmental toxins and corporate‑propagated fragrance additives. It’s no coincidence that the surge in candida‑related dermatoses aligns with the rise of synthetic polymer usage in everyday garments. A discerning individual should therefore scrutinize product ingredient lists and demand transparency from manufacturers.
Vijaypal Yadav
January 3, 2026 AT 19:30Clinically, Candida thrives in hyperglycemic environments, so controlling blood sugar is a foundational step. Topical clotrimazole 1% applied twice daily for two weeks has a success rate exceeding 80 % in intertriginous zones. Adjunctive measures like talc‑free powder reduce moisture, thereby limiting fungal colonization. Lastly, a simple patch‑test can identify contact allergens that perpetuate barrier breakdown.
Ron Lanham
January 22, 2026 AT 14:10There is a moral imperative to approach skin health with both scientific rigor and ethical responsibility. First, we must acknowledge that the human body is an interconnected ecosystem, where fungal overgrowth is seldom an isolated event. Second, the tendency to self‑diagnose using internet images reflects a deeper societal malaise: the erosion of trust in professional expertise. Third, when we neglect the barrier function of the skin, we invite not only Candida but also a host of opportunistic pathogens.
Fourth, the over‑reliance on potent steroids without concurrent antifungal therapy exemplifies a dangerous short‑sightedness that prioritizes immediate symptom relief over long‑term health.
Fifth, the feedback loop described in the article is not merely a biochemical curiosity; it is a clarion call for integrated treatment strategies that address moisture control, barrier repair, and allergen avoidance simultaneously.
Sixth, patients should be educated about the role of diet, as high‑glycemic foods can fuel yeast proliferation, thereby compromising therapeutic outcomes.
Seventh, clinicians ought to prescribe probiotic adjuncts when appropriate, recognizing the gut‑skin axis as a pivotal factor in immune modulation.
Eighth, the healthcare system must facilitate affordable access to diagnostic tools like KOH preparations, lest financial barriers perpetuate misdiagnosis.
Ninth, public health messaging should dispel myths that equate all rashes with infections, thereby reducing stigma and encouraging timely medical consultation.
Tenth, the pharmaceutical industry bears responsibility for ensuring that combination therapies are evidence‑based and not merely profit‑driven.
Eleventh, interdisciplinary collaboration between dermatologists, allergists, and nutritionists can yield comprehensive care plans that respect the complex nature of skin pathology.
Twelfth, patient autonomy must be honored, but it should be informed by accurate, science‑based information rather than anecdotal hearsay.
Thirteenth, we must confront the cultural tendency to prioritize quick fixes over sustainable lifestyle modifications.
Fourteenth, mental health considerations are essential, as chronic skin conditions can precipitate anxiety and depression, which in turn may exacerbate immune dysregulation.
Fifteenth, ultimately, the goal is to break the vicious cycle by addressing both fungal overgrowth and allergic sensitization in tandem, thereby restoring the skin’s natural equilibrium.
Deja Scott
February 10, 2026 AT 08:50In many cultures, skin health is viewed as a reflection of overall well‑being, and traditional remedies often emphasize natural drying agents and barrier restoration. While modern antifungals are effective, integrating gentle, culturally familiar practices-such as using neem leaf extracts or aloe‑based soothing gels-can enhance patient adherence without compromising efficacy. Respecting these customs can also foster a more holistic approach to treatment.