Proton Pump Inhibitors and Antifungals: How They Interfere With Absorption and Effectiveness
 Jan, 27 2026
Jan, 27 2026
Antifungal-PPI Interaction Checker
Check Antifungal-PPI Interaction
Select a proton pump inhibitor and antifungal to see how they interact clinically.
Interaction Summary
Key Clinical Implications
When you’re taking a proton pump inhibitor (PPI) for acid reflux and suddenly need an antifungal for a stubborn infection, things get complicated fast. These two types of drugs don’t just sit quietly in your body-they actively mess with each other. The result? A drug interaction that can make your antifungal treatment fail, even if you’re taking it exactly as prescribed.
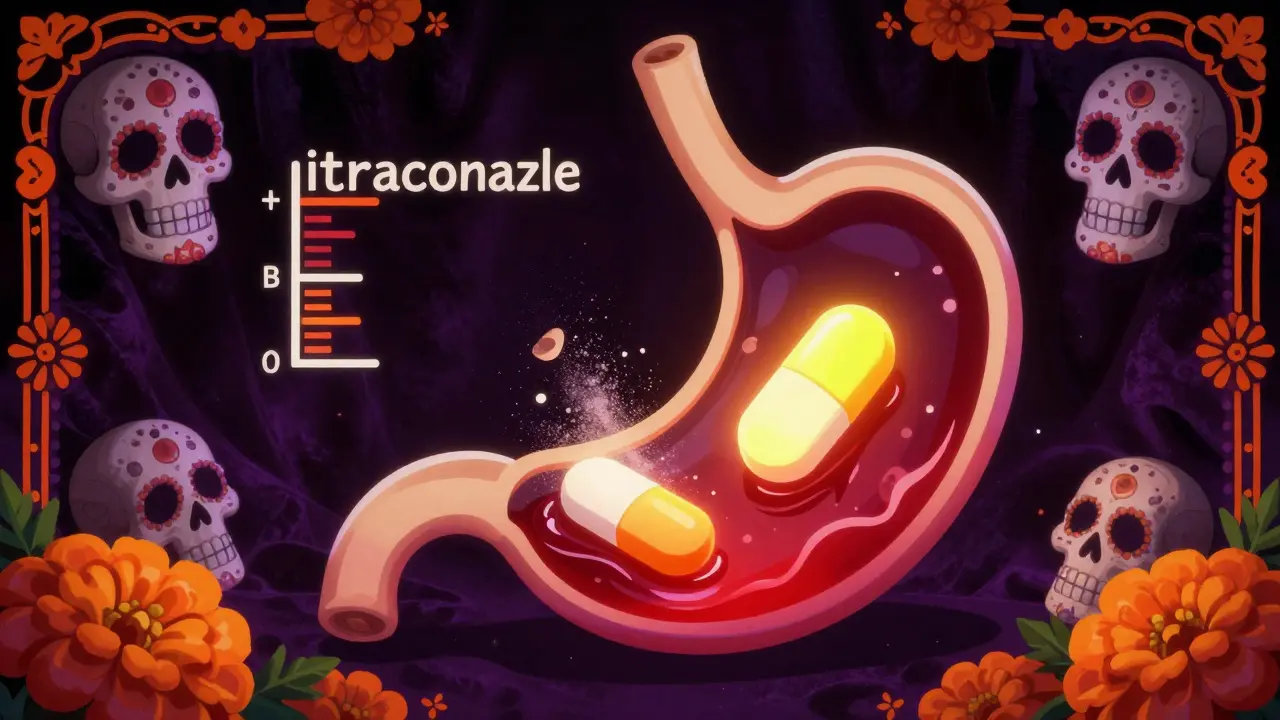
Why Your Antifungal Might Not Work With a PPI
Proton pump inhibitors like omeprazole, pantoprazole, and esomeprazole work by shutting down stomach acid production. That’s great for heartburn, but terrible for certain antifungals. Drugs like itraconazole and ketoconazole need a highly acidic environment to dissolve properly before your body can absorb them. When PPIs raise your stomach pH from around 1.5 to 5 or higher, these antifungals turn into a chalky sludge instead of a usable medicine. A 2023 study in JAMA Network Open tracked 1,243 patients and found that when itraconazole was taken with a PPI, its absorption dropped by 60%. That’s not a small dip-it’s enough to drop blood levels below the minimum needed to kill fungi. The same thing happens with ketoconazole. At pH 1.2, it dissolves at 22 mg/mL. At pH 6.8? Just 0.02 mg/mL. That’s a 1,100-fold drop in solubility.Fluconazole Is the Exception
Not all antifungals play by the same rules. Fluconazole is water-soluble and doesn’t care about stomach acid. Its bioavailability stays steady at 90%±5% whether your stomach is acidic or nearly neutral. The FDA confirmed this in its January 2024 prescribing update. That’s why fluconazole is often the go-to choice when someone’s already on a PPI. But here’s the catch: fluconazole has its own problems. It blocks the liver enzyme CYP2C9, which is how warfarin and some diabetes meds are broken down. If you’re on blood thinners and start fluconazole, your INR can spike dangerously. Dose reductions of 20-30% are often needed. So while fluconazole avoids the absorption issue, it doesn’t escape the interaction game entirely.Voriconazole: A Double-Edged Sword
Voriconazole doesn’t suffer from poor absorption with PPIs, but it gets tangled in a different kind of mess. Both voriconazole and PPIs like pantoprazole are processed by the same liver enzymes: CYP2C19 and CYP3A4. When you take them together, the PPI acts like a traffic jam-slowing down how fast voriconazole gets cleared from your body. A 2015 study in Antimicrobial Agents and Chemotherapy showed this raises voriconazole blood levels by 25-35%. That might sound good, but it’s not. Higher levels mean more side effects: hallucinations, liver damage, vision blurring. The Cleveland Clinic now requires voriconazole blood tests within 72 hours of starting a PPI. Doses often need to be cut by 25-50% to stay safe.
The Paradox: PPIs Might Actually Help Fight Fungi
Here’s where things get weird. A 2024 study published in PMC (PMC10831725) found something unexpected: PPIs like omeprazole might directly weaken fungi. In lab tests, omeprazole blocked a fungal protein called Pam1p-a pump that helps Candida survive stress and resist drugs. When this pump was inhibited, fluconazole became 4 to 8 times more powerful against resistant strains of Candida glabrata. This isn’t just lab magic. It’s a real biological twist: the same drug that steals absorption from itraconazole might make fluconazole work better. Dr. Mahmoud Ghannoum from Case Western Reserve University called this a "therapeutic paradox" in a March 2024 ASM Microbe webinar. Clinical trials are now testing whether adding omeprazole to standard fluconazole can rescue patients with stubborn fungal infections. Phase II trials are underway at Johns Hopkins, with results expected in late 2025.What Doctors Do When Both Drugs Are Needed
In real-world practice, most infectious disease specialists avoid the whole mess. A 2023 survey of 217 pharmacists showed 87% prefer switching to an echinocandin (like caspofungin) instead of trying to time PPIs and azoles around each other. Echinocandins don’t rely on stomach acid or liver enzymes-they’re given by IV and work just fine with PPIs. If you absolutely must use itraconazole or ketoconazole with a PPI, timing matters. UCSF’s protocol says take itraconazole at least two hours before the PPI. Mayo Clinic recommends a 4-6 hour gap for ketoconazole. But even then, absorption still drops from 60% to 45%. That’s not enough. Therapeutic drug monitoring is non-negotiable. For itraconazole, blood levels must stay above 0.5 μg/mL. For voriconazole, aim for 1-5.5 μg/mL.
The Bigger Picture: Why This Matters
PPIs are among the most prescribed drugs in the U.S.-over 124 million prescriptions in 2023. Systemic antifungals aren’t far behind at 15.3 million. About 1 in 5 hospitalized patients gets both. And when they don’t work together? The cost is huge. A 2024 study in JAMA Internal Medicine estimated that bad PPI-azole combos cause $327 million in extra healthcare costs each year from failed treatments, longer hospital stays, and emergency visits. The FDA added a black box warning to itraconazole in June 2023: "Concomitant use with PPIs is contraindicated." The EMA followed in September. Yet a 2024 audit by the Institute for Safe Medication Practices found that over 22% of itraconazole prescriptions in pharmacies were still paired with PPIs. That’s not just ignorance-it’s a systemic failure.What’s Next? New Formulations and Better Options
Scientists aren’t waiting. The FDA’s Antifungal Development Initiative is funding new formulations that bypass stomach acid entirely. One called SUBA-itraconazole uses tiny particles to dissolve regardless of pH. A 2023 Phase I trial showed 92% bioavailability-even with PPIs. That’s a game-changer. Meanwhile, researchers are exploring whether PPIs can be repurposed as antifungal boosters. If the Johns Hopkins trial succeeds, we might soon see omeprazole prescribed not just for heartburn, but to help cure resistant fungal infections. That would turn a problem into a solution. Until then, the message is clear: don’t mix itraconazole or ketoconazole with PPIs. Fluconazole is safer for absorption, but watch for drug interactions with blood thinners. Voriconazole needs close monitoring. And if you’re unsure? Ask your pharmacist. The right choice could mean the difference between healing and a relapse.Can I take fluconazole with a proton pump inhibitor?
Yes, fluconazole can be safely taken with proton pump inhibitors. Unlike itraconazole or ketoconazole, fluconazole doesn’t need stomach acid to be absorbed. Its bioavailability stays above 90% regardless of gastric pH. However, fluconazole can interfere with other medications like warfarin by blocking liver enzymes (CYP2C9), so your doctor may need to adjust those doses.
Why is itraconazole affected by PPIs but not fluconazole?
Itraconazole is highly fat-soluble and requires an acidic stomach environment to dissolve and be absorbed. Proton pump inhibitors raise stomach pH, making it harder for itraconazole to dissolve-leading to up to a 60% drop in absorption. Fluconazole, on the other hand, is water-soluble and absorbs well at any pH, so stomach acidity doesn’t affect it.
Is it safe to take voriconazole with a PPI?
Voriconazole can be taken with a PPI, but it’s risky without monitoring. PPIs slow down how quickly your body clears voriconazole, causing blood levels to rise by 25-35%. This increases the chance of serious side effects like hallucinations or liver damage. Always get a blood test within 72 hours of starting both drugs together, and follow your doctor’s dosing instructions closely.
What should I do if I’m prescribed both a PPI and an antifungal?
Talk to your doctor or pharmacist immediately. If you’re on itraconazole or ketoconazole, switching to fluconazole or an echinocandin like caspofungin is often the safest choice. If you must use itraconazole, take it at least two hours before your PPI, and request therapeutic drug monitoring to check blood levels. Never assume the drugs will work fine together-this interaction can lead to treatment failure.
Are there any new antifungals that don’t interact with PPIs?
Yes. A new formulation called SUBA-itraconazole uses special particles that dissolve without needing stomach acid. In clinical trials, it achieved 92% bioavailability even with PPIs. While not yet widely available, it’s expected to become a standard option in the next few years. Echinocandins like caspofungin are already safe to use with PPIs because they’re given intravenously and don’t rely on stomach absorption.
SRI GUNTORO
January 28, 2026 AT 19:50Wow, so we’re just supposed to trust big pharma’s ‘safe’ alternatives when they’ve been selling us PPIs like candy for decades? Of course fluconazole is ‘safer’-it’s cheaper and doesn’t need fancy monitoring. But let’s not pretend this isn’t just profit-driven medicine pretending to be science. 🤡
Kevin Kennett
January 28, 2026 AT 23:52This is exactly why I tell my patients: ‘Don’t Google your meds, talk to your pharmacist.’ I had a guy come in last week on omeprazole and itraconazole-he thought the ‘antifungal cream’ was enough. We switched him to caspofungin and he’s fungal-free now. Knowledge saves lives, folks.
Howard Esakov
January 30, 2026 AT 21:30Oh please. The FDA’s black box warning? Cute. Meanwhile, in the real world, we’re still prescribing these combos because insurance won’t cover echinocandins. It’s not ignorance-it’s capitalism. 😒
Rhiannon Bosse
February 1, 2026 AT 10:22So let me get this straight-PPIs are making fungi stronger… but also weaker? And now we’re gonna add omeprazole to fluconazole like it’s some kind of magic potion? 🤯 Someone’s getting a Nobel Prize… or a lawsuit. Either way, I’m popcorn-ing.
John Rose
February 2, 2026 AT 00:48Interesting how the science here is so nuanced. The fact that SUBA-itraconazole bypasses gastric pH entirely is a major breakthrough. I hope this formulation gets approved quickly-it could prevent a lot of unnecessary treatment failures. This is the kind of innovation that deserves more attention.
Robert Cardoso
February 2, 2026 AT 13:04You all are missing the forest for the trees. The real problem isn’t the drug interaction-it’s that we’ve turned medicine into a checklist. Doctors don’t think anymore. They just follow guidelines written by committees who’ve never seen a patient with thrush and acid reflux at the same time. This isn’t pharmacology. It’s bureaucratic theater.
matthew martin
February 3, 2026 AT 15:33Man, I love how science flips the script like this. PPIs-villains in one story, secret weapons in another. It’s like finding out your ex is actually the hero of their own movie. Who knew heartburn meds could be antifungal sidekicks? 🤔 The more I learn, the less I feel like I know anything.
Chris Urdilas
February 4, 2026 AT 05:51So if I’m on a PPI and need an antifungal… I’m basically playing Russian roulette with my liver, kidneys, and sanity? Cool. Cool cool cool. 🤪 At least we’ve got a 22% failure rate to keep things spicy. Who needs sleep when you’ve got a 300 million dollar problem?
Jeffrey Carroll
February 4, 2026 AT 23:06Thank you for this comprehensive overview. The data on therapeutic drug monitoring is particularly critical. For clinicians, the key takeaway is not just to avoid combinations, but to implement active surveillance when alternatives are not feasible. This level of detail deserves wider dissemination in medical education.
Phil Davis
February 6, 2026 AT 02:13They say ‘don’t mix meds’… but we do it anyway. Because we’re human. Because we’re tired. Because the system’s broken. And now we’re gonna put a black box warning on it? That’s not safety-that’s liability insurance with a side of guilt.
Irebami Soyinka
February 7, 2026 AT 05:11USA thinks it owns medicine? 😒 In Nigeria, we use neem and turmeric for fungal infections since the 80s. Now you’re playing with lab-made drugs and crying about interactions? We didn’t need FDA to tell us to avoid mixing things. We learned from our grandmas. 🌿🔥
doug b
February 8, 2026 AT 08:43Bottom line: if you’re on a PPI and your antifungal isn’t working, don’t blame yourself. Blame the system. Talk to your pharmacist. Ask about echinocandins. You’ve got options. Don’t give up.
Mel MJPS
February 9, 2026 AT 22:54My aunt was on this combo and got really sick. We didn’t know it was the meds. She’s fine now, but it scared the hell out of us. Thanks for explaining this so clearly. I’m sharing this with my whole family.
Katie Mccreary
February 10, 2026 AT 06:53Wait-so PPIs are secretly helping fluconazole? That means someone’s been lying about ‘safe’ antifungals for years. Who’s funding these trials? Who’s hiding the data? I’m not just curious-I’m suspicious.