Common Pharmacy Dispensing Errors and How to Prevent Them
 Dec, 6 2025
Dec, 6 2025
Every year, millions of patients receive the wrong medication, the wrong dose, or a drug that interacts dangerously with something they’re already taking. These aren’t hypothetical risks-they’re real, frequent, and often preventable. In community and hospital pharmacies around the world, dispensing errors happen at a rate of about 1.6% of all prescriptions filled. That might sound small, but when you’re talking about hundreds of thousands of prescriptions daily, it adds up to thousands of patients getting harmed-not because of bad intentions, but because of broken systems.
What Are the Most Common Dispensing Errors?
Not all mistakes look the same. Some are obvious, like handing a patient insulin when they were prescribed metformin. Others are quieter, more dangerous, and harder to catch. The top three errors reported by pharmacy safety experts are:- Wrong medication, strength, or form (32% of all errors): This includes giving amoxicillin instead of azithromycin, 500mg instead of 250mg, or tablets instead of liquid for a child who can’t swallow pills.
- Dose miscalculations (28%): Especially common with pediatric, elderly, or kidney-impaired patients. A simple math error in weight-based dosing can turn a safe dose into a toxic one.
- Missing drug interactions or contraindications (24%): Giving warfarin to someone already on an NSAID like ibuprofen, or prescribing an SSRI with an MAOI, can lead to life-threatening bleeding or serotonin syndrome.
Other frequent errors include dispensing expired meds, giving the wrong duration (like 30 days instead of 7), or misreading handwritten scripts. One hospital pharmacist in Adelaide told me last year that they once dispensed vancomycin as an IV push instead of an infusion-resulting in severe flushing and hypotension. That’s not rare. It’s called “Red Man Syndrome,” and it’s preventable.
Some drugs are just more dangerous when messed up. Anticoagulants like warfarin and heparin show up in 31% of serious error cases. Opioids, antimicrobials, and anticonvulsants are also high-risk. In fact, nearly half of all antibiotic-related errors happen because the pharmacist didn’t check the patient’s allergy history.
Why Do These Errors Keep Happening?
It’s easy to blame the pharmacist. But the real problem isn’t people-it’s pressure, process, and poor design.- Workload pressure is the #1 cause. Pharmacies are stretched thin. One pharmacist in a busy urban clinic told me they’re expected to dispense 200+ prescriptions a day, with only 2 minutes per script. That’s not enough time to catch a typo.
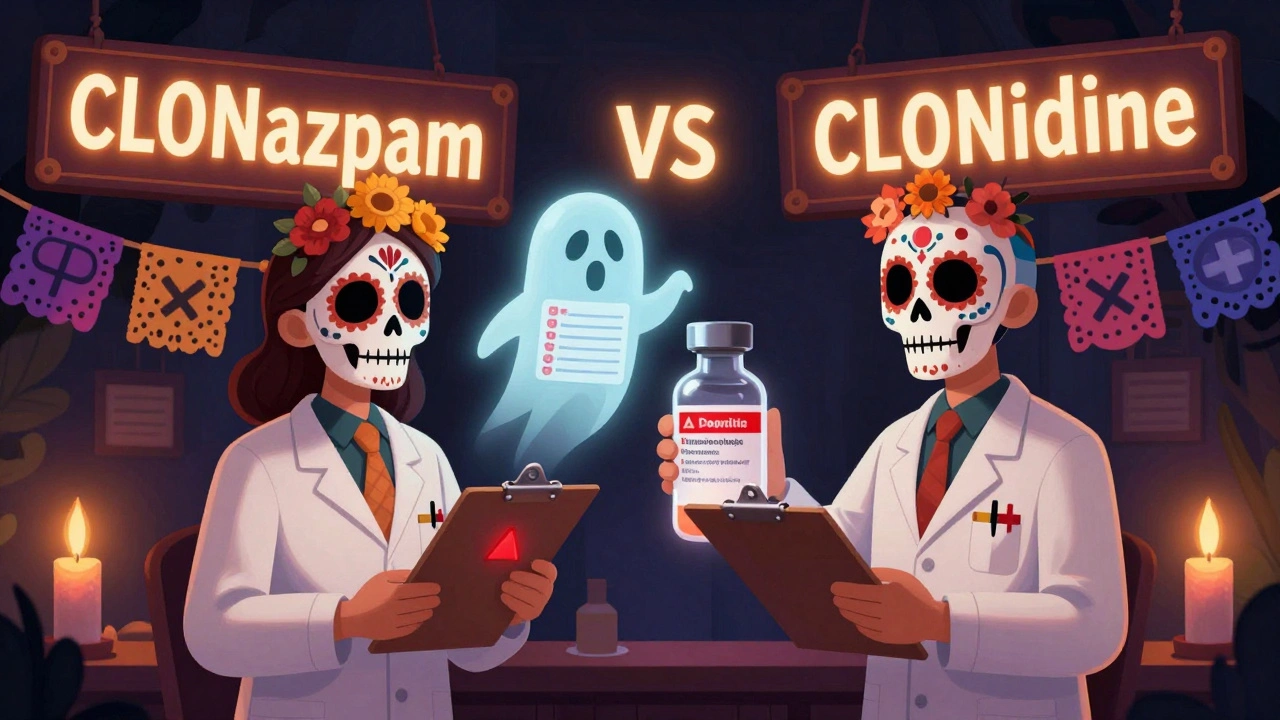
- Similar drug names trip people up constantly. Look at hydroxyzine and hydralazine. Or clonazepam and clonidine. Even small spelling differences get missed when you’re rushing.
- Interruptions are deadly. If you’re verifying a prescription and someone asks you for a refill, your brain resets. Studies show that just three interruptions per prescription increase error risk by over 12%.
- Illegible handwriting still causes 43% of errors-even in 2025. Electronic prescriptions help, but not every doctor uses them.
- Missing patient info is a silent killer. If you don’t know the patient’s kidney function, weight, or current meds, you’re guessing. And guessing kills.
Verbal prescriptions are another minefield. When a nurse calls in a drug name like “Lortab” instead of “Lorazepam,” the pharmacist hears what they expect-not what’s said. Sound-alike names cause 22% of errors in phone orders.
How to Stop These Errors Before They Happen
The good news? Most of these errors can be prevented with simple, proven systems. It’s not about hiring more staff or working harder. It’s about designing better workflows.1. Use Barcode Scanning
Barcoding is the single most effective tool in modern pharmacies. When a pharmacist scans the medication and the patient’s wristband, the system checks: Is this the right drug? Right dose? Right patient? Right time? A 2021-2023 survey of 127 hospitals found barcode systems cut dispensing errors by 47.3%. Wrong drug errors dropped by over 52%. Wrong dose by nearly 49%.2. Implement Double Checks for High-Risk Drugs
Insulin, heparin, opioids, and chemotherapy drugs need two sets of eyes. One pharmacist prepares it. A second verifies it. No exceptions. One hospital in South Australia reported a 78% drop in insulin errors after implementing this rule. It’s not extra work-it’s a safety net.3. Use Tall Man Lettering
This isn’t fancy tech. It’s just capitalizing key letters to make similar names stand out. Instead of writing “Hydralazine,” write “HYDRAZINE.” Instead of “Clonazepam,” write “CLONazepam.” It sounds small, but 214 community pharmacies that adopted this saw a 56.8% drop in look-alike/sound-alike errors.4. Verify Allergies Every Single Time
Don’t rely on memory. Don’t assume the chart is up to date. Every time you dispense an antibiotic, anticonvulsant, or NSAID, cross-check the allergy list. In one audit, 41% of antibiotic errors happened because the pharmacist didn’t check. That’s not negligence-it’s a system failure. Make allergy checks mandatory and automated.5. Use Clinical Decision Support Tools
Your pharmacy software should flag interactions, renal dosing issues, and duplicate therapies. But here’s the catch: too many alerts cause alert fatigue. A 2023 study found that when systems bombarded pharmacists with 15+ pop-ups per script, they started ignoring them. The solution? Smart alerts. Only trigger warnings for high-risk interactions-like warfarin with fluconazole, or SSRIs with tramadol.6. Standardize and Document Everything
If a patient gets a new prescription, document the reason, the dose, and the instructions clearly. If a drug is discontinued, update the list. If a lab value changes (like creatinine), make sure it’s visible at the point of dispensing. One pharmacy chain reduced errors by 38.7% in a year just by making their digital records more complete.What’s Not Working-and Why
Not every fix is a miracle. Some tech solutions create new problems.- Computerized Prescribing (CPOE) reduces errors by 43%, but introduces new ones in 17.8% of cases. Why? Because doctors pick the wrong drug from a dropdown, or the system auto-fills the wrong dose. It’s not the tech-it’s the design.
- Robotic dispensers are fast and accurate, but cost $150,000 to $500,000. Most community pharmacies can’t afford them.
- AI prediction tools are promising-they’ve cut errors by over 50% in pilot studies-but they’re still in testing. They’re not ready for widespread use yet.
And here’s the biggest barrier: cost and training. Over two-thirds of pharmacies say new systems are too expensive. Nearly half say staff aren’t trained well enough to use them. Without buy-in from leadership and proper training, even the best tools fail.

What You Can Do as a Patient
You’re not powerless. You’re the last line of defense.- Always check the label before leaving the counter. Does the name match your prescription? Does the dose look right?
- Ask: “Is this the same as last time?” If it looks different, speak up.
- Keep a current list of all your meds-including supplements-and bring it to every visit.
- If you’re given a new drug, ask: “What’s this for? What are the side effects? What should I avoid?”
One woman in Adelaide caught a dangerous interaction after her pharmacist gave her a new antidepressant. She remembered her doctor warned her not to take it with St. John’s Wort. She asked the pharmacist: “Did you see this on my list?” He hadn’t. He checked the system. It was missing. He corrected it before she left.
The Future Is Better Systems, Not Better Pharmacists
The truth is, no pharmacist is perfect. We’re human. We get tired. We get distracted. The goal isn’t to find the flawless pharmacist. It’s to build a system that doesn’t rely on perfection.The World Health Organization and the Institute for Safe Medication Practices are working on a global standard for reporting medication errors. By 2025, every pharmacy should be using the same categories to track mistakes. That means we’ll finally know what’s working-and what’s not.
Until then, the best defense is simple: slow down, double-check, speak up. And if you’re a pharmacist? Advocate for better tools, better training, and better support. You’re not the problem. You’re the solution.
Louis Llaine
December 8, 2025 AT 01:04So let me get this straight - we’re blaming pharmacists for not catching errors when they’re expected to do 200 scripts a day like they’re some kind of pharmacy robot? Cool. I’ll just sit here with my 12 medications and hope the guy behind the counter isn’t on his 187th script while his kid’s crying in the back.
Ted Rosenwasser
December 8, 2025 AT 10:53The real issue is systemic pharmacokinetic negligence compounded by inadequate CPOE interface design. Barcoding reduces errors by 47.3%? That’s statistically significant, yes - but only if you control for confounding variables like workflow entropy and cognitive load thresholds. The WHO’s 2025 standardization initiative will fail without a Bayesian error prediction model integrated into EHRs. Also, Tall Man Lettering is a Band-Aid on a hemorrhage.
Ashley Farmer
December 8, 2025 AT 20:47I’ve been a patient for over 20 years and I’ve had two near-misses. The first time, I didn’t say anything because I was scared to seem like a hassle. The second time, I asked, ‘Is this the same as last month?’ and they caught it. I wish more people knew it’s not rude to ask - it’s saving your life. You don’t need to be loud. Just be clear. ‘This looks different.’ That’s all it takes.
Kyle Flores
December 10, 2025 AT 11:39my grandma got the wrong blood pressure med last year and almost went to the er. she didnt even notice until her neighbor pointed out the bottle looked different. nobody checks labels anymore. we just grab and go. but like... if you're on 10 pills a day, how are you supposed to remember what each one looks like? the system is broken, not the people.
Ryan Sullivan
December 11, 2025 AT 06:00Let’s be brutally honest: 90% of dispensing errors stem from incompetent prescribers who can’t spell, write legibly, or understand basic pharmacology. The pharmacist is the last line of defense against a cascade of clinical incompetence. And yet, we treat them like glorified cashiers. Meanwhile, doctors get paid millions to write scripts they don’t understand. The real tragedy isn’t the error - it’s the culture that normalizes it.
Wesley Phillips
December 12, 2025 AT 12:43barcoding is the only thing that matters tbh 🤖💊
also i once got metformin instead of metoprolol and i was like... wait why am i so calm right now? 🤔
Olivia Hand
December 13, 2025 AT 15:59How many of these errors are documented in public databases? I’ve read the WHO report - but I can’t find any real-time tracking. If pharmacies aren’t required to log every near-miss, how do we know if these ‘solutions’ are actually working? Or are we just pretending to fix things while the pressure keeps building?
Desmond Khoo
December 13, 2025 AT 16:29you guys are so right about the double-check thing - my cousin works at a pharmacy and they started doing it for insulin and now she actually goes home without crying every day 😭
it’s not magic, it’s just... respect. give people time. give them space. they’re not machines.
Sam Mathew Cheriyan
December 15, 2025 AT 03:38barcodes? double checks? pfft. the real problem is the government forcing pharmacies to use big pharma’s software. they want you to give the wrong med so you have to come back and buy more. it’s all a scam. i saw a doc on youtube that said the FDA approves drugs with errors on purpose. they need the sales.
Ernie Blevins
December 16, 2025 AT 15:00pharmacists are overpaid. they make 120k and still mess up. if you can’t handle 200 scripts a day, get a different job. people die because you’re lazy. end of story.