Antihistamines and Dementia Risk: What Older Adults Need to Know
 Dec, 7 2025
Dec, 7 2025
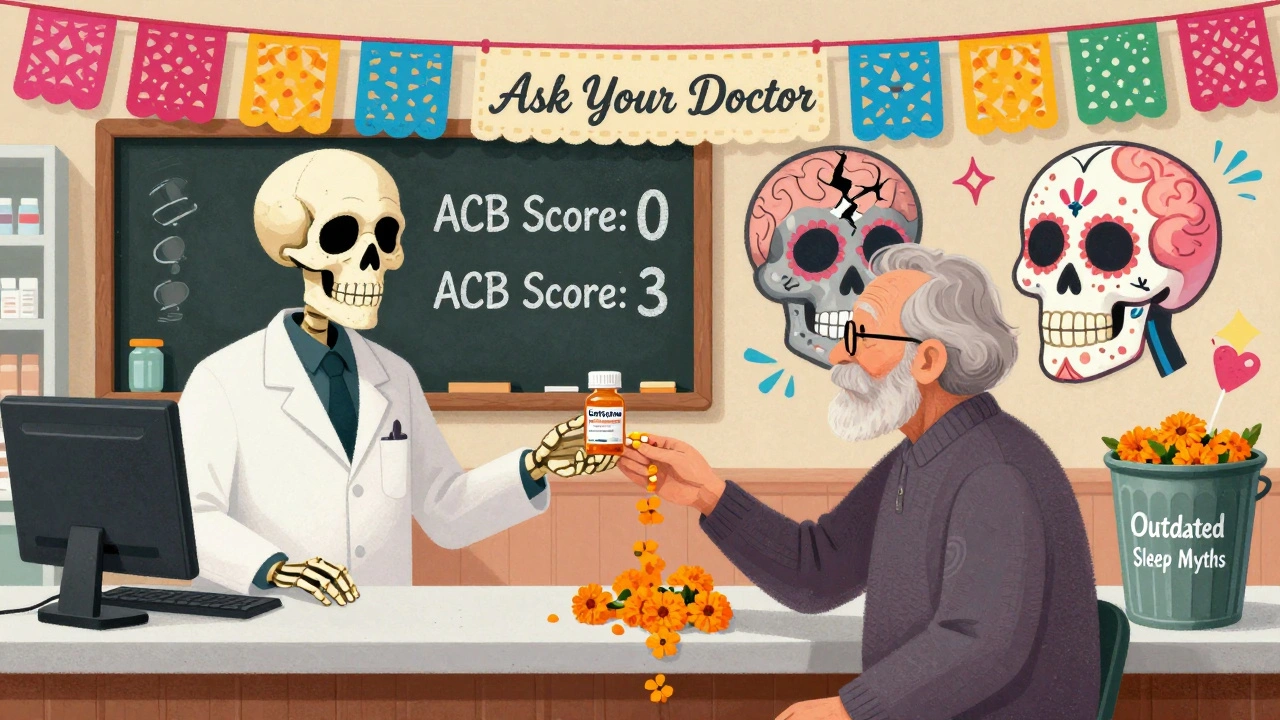
Anticholinergic Burden Calculator
What is Anticholinergic Burden?
Anticholinergic drugs block acetylcholine, a brain chemical important for memory and cognition. The Anticholinergic Cognitive Burden (ACB) Scale rates drugs from 0 (no anticholinergic effect) to 3 (strongest effect). This calculator helps you understand your total anticholinergic burden from medications.
Many older adults reach for diphenhydramine-commonly sold as Benadryl-to help them sleep or ease allergy symptoms. It’s cheap, easy to find, and works fast. But what if that little white pill could be quietly affecting the brain? Over the past decade, research has raised serious questions about long-term use of first-generation antihistamines and their link to dementia. The truth isn’t simple. Some studies say yes, others say no. But one thing is clear: if you’re over 65 and taking these meds regularly, it’s time to ask questions.
Why First-Generation Antihistamines Are Different
Not all antihistamines are created equal. There are two main types: first-generation and second-generation. The difference isn’t just about how strong they are-it’s about where they go in your body. First-generation antihistamines like diphenhydramine, doxylamine, and chlorpheniramine cross the blood-brain barrier easily. Once inside, they block acetylcholine, a chemical your brain needs to form memories and stay sharp. This is called anticholinergic activity. Think of it like turning down the volume on a key part of your brain’s communication system. That’s why these drugs make you drowsy. But over years, that same effect might wear down cognitive function. Second-generation antihistamines-like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra)-were designed differently. They don’t cross into the brain as easily. They’re still great for allergies, but they don’t mess with your memory the same way. Their anticholinergic effect is 100 to 1,000 times weaker than the first-gen versions.The Evidence: Mixed, But the Warning Signs Are Real
In 2015, a major study in JAMA Internal Medicine followed over 3,400 people aged 65 and older for more than 10 years. It found that people who took anticholinergic drugs-especially antidepressants, bladder meds, and antipsychotics-had a higher risk of dementia. But when they looked at antihistamines alone? No clear link. That study didn’t rule out antihistamines entirely. It just said the risk wasn’t as strong as with other drug classes. A 2022 study of nearly 9,000 older adults found that those using first-gen antihistamines had a slightly higher rate of dementia (3.83%) compared to those using second-gen (1.0%). But when researchers adjusted for other factors like age, health conditions, and sleep problems, the difference wasn’t statistically significant. Here’s the catch: other studies that grouped all anticholinergic drugs together-antihistamines, bladder meds, antidepressants-did show a 46% higher dementia risk with long-term use. That’s where the confusion comes from. Are antihistamines the problem? Or are they just hanging out with riskier drugs? The American Geriatrics Society doesn’t wait for perfect data. Their 2023 Beers Criteria, updated in June 2023, says first-gen antihistamines should be avoided in adults 65+. That’s a Level A recommendation-the strongest possible. They don’t say it’s proven. They say the risk is too high to ignore.What About Sleep? The Hidden Trap
Most people don’t take diphenhydramine for allergies. They take it to sleep. A 2022 survey by the National Council on Aging found that 42% of adults over 65 use over-the-counter antihistamines as a sleep aid. And 78% of them had no idea these drugs have anticholinergic effects. They think it’s just a “natural” sleep aid because it’s sold next to melatonin. But here’s the problem: antihistamines don’t improve sleep quality. They just make you drowsy. That’s not the same as restorative sleep. And over time, your brain adapts. You need more to get the same effect. You might start taking it every night. Then every other night. Then you wonder why you’re foggy in the morning. One Reddit user, a geriatric care manager with 2,400 karma, wrote in March 2023: “83% of my clients over 70 are on Benadryl nightly. None of them know it’s an anticholinergic. They think it’s harmless.”
What’s the Real Risk? The Numbers Don’t Lie, But They Don’t Tell the Whole Story
Let’s look at the data. The Anticholinergic Cognitive Burden Scale (ACB) rates drugs on a scale from 0 to 3. Diphenhydramine? Level 3-the highest. That means it’s one of the most potent anticholinergics you can take without a prescription. Fexofenadine? Level 0. No anticholinergic effect at all. The Choosing Wisely campaign, led by the American Board of Internal Medicine, lists “avoid diphenhydramine for chronic insomnia in older adults” as one of its top five recommendations for geriatric care. That’s not a suggestion. It’s a call to action. But here’s what’s missing from the headlines: correlation isn’t causation. People who take diphenhydramine long-term often have other issues-chronic allergies, depression, insomnia, or even early signs of cognitive decline. Maybe they’re taking the drug because their brain is already struggling. Maybe the drug is making it worse. Or maybe it’s both. A 2023 analysis from the UK Biobank found no link between antihistamine use and dementia when researchers accounted for underlying sleep disorders. That suggests the real culprit might not be the drug-it’s the condition the drug is trying to treat.What Should You Do? Practical Steps for Safer Choices
You don’t have to panic. But you do need to act.- Check your meds. Look at the active ingredient. If it’s diphenhydramine, doxylamine, or chlorpheniramine, you’re on a first-gen antihistamine.
- Switch to second-gen. Try loratadine, cetirizine, or fexofenadine for allergies. They work just as well without the brain fog.
- Ditch it for sleep. Don’t use antihistamines as a nightly sleep aid. There are better, safer options.
- Ask about CBT-I. Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold standard for chronic sleep problems. Studies show it works for 70-80% of older adults. It’s not magic, but it’s effective-and it doesn’t mess with your brain chemistry.
- Review meds every six months. If you’re on multiple prescriptions, ask your doctor or pharmacist to run an anticholinergic burden check. Many pharmacies now offer this service for free.
Alternatives That Actually Work
If you’re struggling with sleep, here’s what works better than Benadryl:- CBT-I: Talk therapy that rewires your brain’s sleep patterns. No pills. No side effects.
- Low-dose doxepin (Silenor): A prescription sleep aid with minimal anticholinergic activity (ACB score of 1). Approved for insomnia since 2010.
- Melatonin: A natural hormone that helps regulate sleep cycles. Safe for short-term use.
- Good sleep hygiene: Dark room, cool temperature, no screens before bed, consistent schedule.
Why This Matters More Than You Think
We’re living longer. But longer life shouldn’t mean longer decline. Every year, millions of older adults take medications that were never meant for daily, long-term use. Antihistamines are one of the most common examples. The pharmaceutical industry has shifted. First-gen antihistamine sales dropped 23.7% between 2015 and 2022. Second-gen sales rose 18.4%. Why? Because people are learning. Doctors are warning. Pharmacies are updating labels. The European Medicines Agency now requires all antihistamine packaging to include a warning about “potential long-term cognitive effects with prolonged use.” The FDA hasn’t done the same for over-the-counter products-but they’re reviewing all anticholinergics as of 2023. The message isn’t: “Stop taking Benadryl.” It’s: “Know what you’re taking. Ask if it’s still necessary. Look for safer alternatives.”When to Talk to Your Doctor
You should bring this up if:- You’ve been taking diphenhydramine or similar drugs for more than 3 months
- You feel foggy, forgetful, or confused after taking them
- You’re taking more than one anticholinergic drug (e.g., Benadryl + a bladder med)
- You’re having trouble sleeping and rely on OTC meds
Final Thought: It’s Not About Fear. It’s About Awareness.
There’s no smoking gun. No single study proves that Benadryl causes dementia. But there’s enough warning to make you pause. For older adults, the brain is more sensitive. The body processes drugs slower. Small risks add up. You don’t have to stop using antihistamines. But you do have to choose wisely. And you deserve to know what you’re putting in your body. The safest choice isn’t always the cheapest. But it’s the one that keeps your mind clear-for years to come.Do all antihistamines increase dementia risk?
No. Only first-generation antihistamines like diphenhydramine (Benadryl), doxylamine, and chlorpheniramine have strong anticholinergic effects linked to potential cognitive risks. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have minimal to no anticholinergic activity and are considered safe for long-term use in older adults.
Is it safe to take Benadryl occasionally?
Taking Benadryl once in a while-for a bad allergy reaction or a single night of poor sleep-is unlikely to cause harm. The concern is daily or near-daily use over months or years. The cumulative effect of blocking acetylcholine over time may contribute to cognitive decline in vulnerable individuals, especially those over 65.
What are the best alternatives to Benadryl for sleep?
The most effective long-term solution is Cognitive Behavioral Therapy for Insomnia (CBT-I), which has been shown to work for 70-80% of older adults. For short-term help, low-dose melatonin or prescription low-dose doxepin (Silenor) are safer options than antihistamines. Always talk to your doctor before starting any new sleep aid.
Can I switch from Benadryl to Claritin for allergies?
Yes. Claritin (loratadine) is a second-generation antihistamine that treats the same allergy symptoms as Benadryl without crossing into the brain or blocking acetylcholine. It doesn’t cause drowsiness in most people and is safe for daily use. Many pharmacists recommend this switch for older adults.
Why do doctors still prescribe Benadryl if it’s risky?
Many doctors know the risks, but patients often ask for it because it’s familiar, cheap, and works quickly. Some older patients have been taking it for decades without realizing the potential long-term effects. Also, not all providers are up to date on the latest guidelines. That’s why it’s important for patients to ask questions and bring a full list of medications to appointments.
Are there any tests to check if antihistamines are affecting my brain?
There’s no single blood test or scan that shows anticholinergic brain impact. But your doctor can assess cognitive function with simple tests like the MoCA (Montreal Cognitive Assessment). They can also calculate your total anticholinergic burden using tools like the Anticholinergic Cognitive Burden Scale (ACB). If you’re on multiple medications, ask for a medication review-many pharmacies offer this for free.
ian septian
December 8, 2025 AT 03:53Switch to Zyrtec. Done.
Lola Bchoudi
December 9, 2025 AT 12:49As a geriatric pharmacist, I see this daily. First-gen antihistamines are a silent epidemic in senior households. The ACB score isn't just a number-it's a clinical red flag. Diphenhydramine’s Level 3 anticholinergic burden is clinically equivalent to some antipsychotics used in dementia. And yet, it's still on the nightstand next to the reading glasses. The real tragedy? Most patients aren't even aware they're taking it-multiple OTC products contain it under aliases like 'PM pain reliever' or 'sleep aid.' We need better labeling, better counseling, and better awareness. It's not about fear. It's about pharmacovigilance.
Morgan Tait
December 9, 2025 AT 20:11Let me tell you something they don't want you to know... Big Pharma *wants* you to be confused. They made second-gen drugs more expensive so you'd stick with Benadryl. Why? Because dementia means long-term care contracts. And long-term care? That's where the real money is. They've been pushing these anticholinergics for decades-while quietly funding studies that 'find no link.' You think the FDA's slow to act? They're getting paid. Check the revolving door between pharma lobbyists and the FDA. This isn't science-it's profit-driven obfuscation. Wake up. The pills are poison. And they're selling you the cure… in a different bottle.
Darcie Streeter-Oxland
December 11, 2025 AT 02:23It is, of course, imperative to acknowledge the methodological limitations inherent in the longitudinal studies referenced. The confounding variables-particularly the presence of comorbid sleep disorders and depression-are not adequately controlled for in the majority of these analyses. Furthermore, the reliance on self-reported medication use introduces significant recall bias. While the American Geriatrics Society’s recommendation is prudent, it cannot be construed as conclusive evidence of causation. A more rigorous, double-blind, placebo-controlled trial would be necessary to substantiate the purported link.
Sarah Gray
December 12, 2025 AT 09:05Anyone who still uses diphenhydramine after 65 is either willfully ignorant or has been misled by the pharmaceutical-industrial complex. It’s not ‘just Benadryl.’ It’s neurochemical sabotage. And if you’re using it for sleep, you’re not sleeping-you’re chemically sedating your hippocampus into oblivion. There’s no excuse. You have access to PubMed. You have a smartphone. You have a pharmacist down the street. Choose better. Or don’t. But don’t pretend you didn’t know.
Kathy Haverly
December 12, 2025 AT 22:38Oh, so now we’re blaming the drug? What about the fact that people who take Benadryl nightly are the same ones who eat processed food, sit all day, drink caffeine until midnight, and never see sunlight? You think the pill’s the problem? It’s the entire lifestyle. This is just another way for medical elites to shame the elderly into compliance. ‘Stop taking Benadryl’-sure. But fix their housing. Fix their loneliness. Fix their 3 a.m. panic attacks. Then maybe they won’t need it. But nope. Let’s just blame the $5 bottle.
Andrea Petrov
December 13, 2025 AT 08:24I’ve been reading about this for years. And I’m not paranoid-I’m informed. The FDA has known since 2018 that anticholinergics cause brain shrinkage in MRI scans. They just won’t admit it because the lawsuits would bankrupt them. I checked my own meds. Benadryl. Zyrtec. My blood pressure pill. My bladder med. All Level 2 or 3. I’m not dying of dementia-I’m being slowly erased. And no one’s coming to help. Not my doctor. Not my kids. Just me and my pill organizer. I’m 72. I’ve taken this stuff for 30 years. Now I’m scared. But no one listens. So I just keep taking it. Because what else can I do?
Steve Sullivan
December 13, 2025 AT 14:50bro. i get it. benadryl makes you sleepy. but so does being tired from work, stress, bad sleep hygiene, etc. maybe the real issue isn't the drug-it's that we've stopped teaching people how to sleep. cbt-i is the real MVP here. also, if you're over 65 and still using benadryl, you're probably not doing the other stuff either. go for a walk. turn off the screen. drink water. cool room. it's not magic. it's just basic. but nobody wants to do basic. they want a pill. 🤷♂️💊
George Taylor
December 15, 2025 AT 10:02...and yet... the studies... are... inconclusive... (period). The 2022 paper... adjusted for... confounders... and found... no significant difference... (period). The ABA... is... overreaching... (period). The Beers Criteria... is... based on... association... not causation... (period). Why... are... we... demonizing... a... $3... OTC... medication... when... the... real... culprits... are... loneliness... and... poor... nutrition... (period)?
Nikhil Pattni
December 15, 2025 AT 19:36Actually, in India, we have a different problem-people take Benadryl for fever, for cough, for cold, for allergy, for sleep, for anxiety, even for motion sickness. And they take it daily. No one checks the label. No one knows what anticholinergic means. My grandmother took it for 20 years. She’s 80 now, and she forgets where she put her slippers. But she says, ‘It’s just Benadryl, beta.’ We don’t have geriatric pharmacists. We don’t have warning labels. We don’t even have a proper healthcare system. So yes, the drug is dangerous, but the system that lets people take it without oversight? That’s the real monster. I tried to explain this to my uncle-he said, ‘If it works, why change?’ And honestly? I don’t blame him.
William Umstattd
December 17, 2025 AT 17:05They call it ‘Benadryl’ like it’s a friend. Like it’s harmless. Like it’s grandma’s little helper. But it’s not. It’s a chemical ghost-stealing your memories, one night at a time. And for what? A few extra hours of unconsciousness? You think you’re sleeping? No. You’re being drugged into a fog that never lifts. And when your mind starts to slip? You’ll blame age. You’ll blame stress. You won’t blame the little white pill you’ve been swallowing like candy. Shame on you. Shame on all of us for letting this happen.
Simran Chettiar
December 18, 2025 AT 13:55It is a profound paradox that in an era of unprecedented medical advancement, we continue to rely on pharmacological interventions that are both archaic and potentially neurotoxic. The persistence of first-generation antihistamines in geriatric practice reflects not merely a failure of education, but a systemic collapse in the ethical imperative to prioritize cognitive preservation over transient symptomatic relief. One cannot help but observe that the commodification of sleep and allergy relief has rendered the human brain an expendable organ in the calculus of convenience. The true tragedy lies not in the pharmacology, but in the cultural normalization of cognitive erosion as an inevitable consequence of aging.
Anna Roh
December 20, 2025 AT 13:27Okay but what about melatonin? I’ve been taking 3mg every night for 5 years and I feel fine. Is that worse? Also, my cousin’s doctor switched her to Zyrtec and now she’s super dizzy. So maybe it’s not that simple? I don’t know. I’m just tired.
Richard Eite
December 21, 2025 AT 12:01