Pill Splitting: What You Need to Know About Safety, Risks, and When It Works
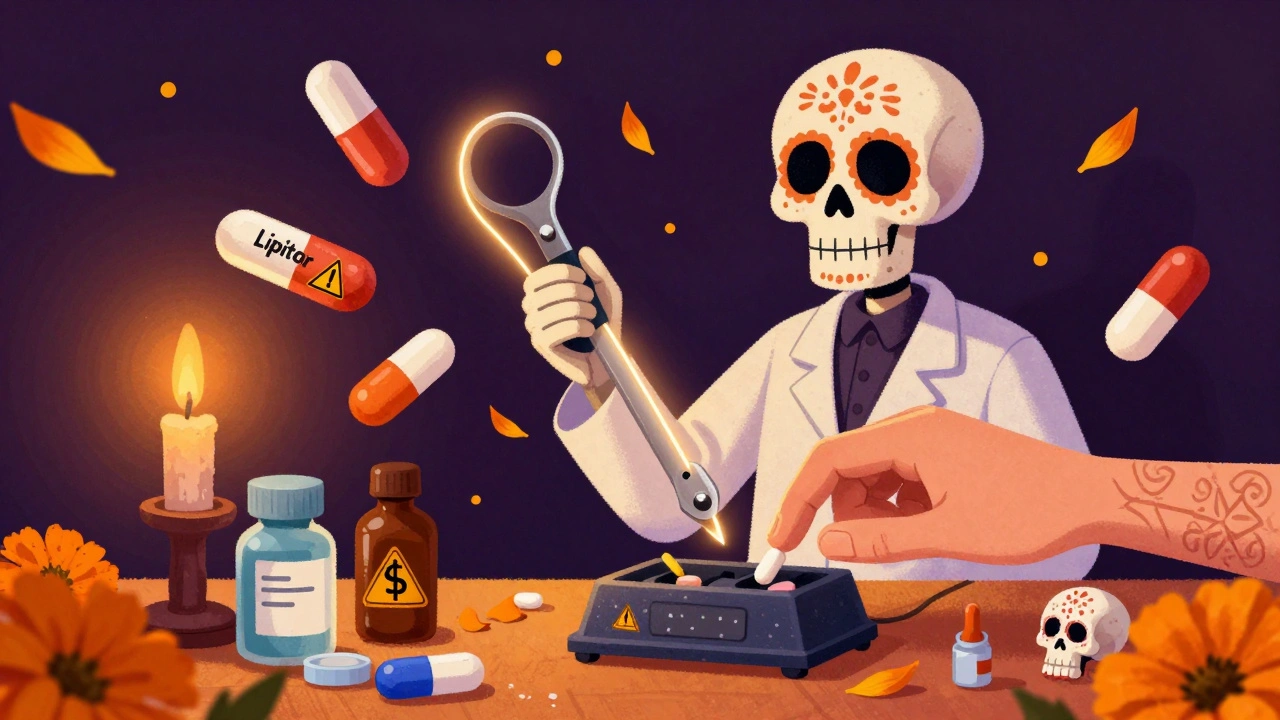
When you split a pill, you're not just cutting a tablet in half—you're changing how your body gets the medicine. pill splitting, the practice of dividing a tablet or capsule to adjust dosage. Also known as tablet splitting, it's a common way people stretch their prescriptions, especially with expensive or high-dose meds. But not all pills are made to be split. Some break unevenly, some lose potency, and others can be downright dangerous if split incorrectly.
Take narrow therapeutic index, drugs where even a small change in dose can cause harm or reduce effectiveness medications like warfarin, levothyroxine, or cyclosporine. These aren’t just any pills. A 10% difference in dose can lead to a blood clot, thyroid crash, or organ rejection. That’s why 27 U.S. states have laws blocking pharmacists from swapping these for generics without your doctor’s OK. Splitting them? Even riskier. You’re not just guessing the dose—you’re gambling with your health.
Then there’s the generic drugs, lower-cost versions of brand-name medicines that must meet FDA standards for safety and effectiveness. They’re great for saving money—up to 80% off in some cases—but they’re not all the same. Some generics have different fillers, coatings, or release mechanisms. Splitting a generic extended-release pill might turn it into a fast-release one, flooding your system with too much drug at once. That’s why recalls happen. And why you need to know what’s inside that tablet before you grab the pill splitter.
Some pills are designed to be split—scored tablets, like certain statins or blood pressure meds. Others? Never. Capsules, enteric-coated pills, time-release formulas, or anything with a hard shell should stay whole. If your pill doesn’t have a visible line down the middle, don’t assume it’s safe. Ask your pharmacist. Look up the drug’s prescribing info. Or better yet, ask your doctor if a lower-dose version is available. It’s often cheaper and safer than splitting.
And here’s the thing: pill splitting isn’t just about cost. It’s about control. People split pills because they can’t afford the full dose, because their insurance won’t cover the lower strength, or because their doctor didn’t offer alternatives. But if you’re splitting meds for chronic conditions like heart disease, epilepsy, or thyroid issues, you’re playing with fire. One study found that patients who split pills for anticoagulants had a 30% higher chance of dangerous bleeding events. That’s not a risk worth taking.
What you’ll find in the posts below are real-world stories and data-driven checks on what works—and what doesn’t. From why some generics cause rejection in transplant patients, to how state laws block risky substitutions, to how food and timing change how your split pill behaves. No fluff. No guesswork. Just what you need to know before you cut that tablet.

Pill Splitting Safety: Which Medications Are Safe to Split and Which Are Not
Learn which pills are safe to split for cost savings or easier swallowing-and which ones can be dangerous. Get clear guidelines on safe techniques, risky medications, and smarter alternatives.
How to Avoid Contamination When Splitting or Crushing Pills: A Safe, Step-by-Step Guide
Learn how to safely split or crush pills without risking contamination, inaccurate dosing, or exposure to hazardous drugs. Follow proven steps, use the right tools, and know which pills should never be touched.