Medication Contamination: What It Is, Why It Happens, and How to Stay Safe
When you swallow a pill, you expect it to do what it’s supposed to—without anything extra. But medication contamination, the presence of unintended substances in pharmaceutical products happens more often than most people realize. It’s not always about dirty factories. Sometimes it’s a chemical leftover from another drug, a mold spore in a batch, or even tiny metal particles from faulty equipment. These aren’t theoretical risks—they’ve pulled drugs off shelves, sent patients to the hospital, and led to recalls that affect thousands.
Generic drug recalls, often tied to contamination from overseas manufacturing make up a large chunk of these incidents. The same active ingredient might be in your bottle as in the brand-name version, but if the facility doesn’t follow strict cleanroom standards, the results can be dangerous. Drug contamination, whether from unclean equipment, poor storage, or cross-contamination during production doesn’t always show up in lab tests right away. That’s why some recalls happen months after the pills are sold. And when it comes to critical meds like immunosuppressants or blood thinners, even tiny changes in purity can cause rejection, clots, or seizures.
The FDA drug recalls, public warnings issued when medications are found unsafe or contaminated aren’t just paperwork—they’re lifesavers. But they don’t always come fast enough. Many people don’t know their meds were part of a recall until they see a news alert or their pharmacy calls. That’s why understanding the signs matters: unusual color, smell, or texture in your pills? A sudden side effect you’ve never had before? These aren’t just bad luck—they could be red flags.
Contamination isn’t always about the drug itself. Sometimes it’s the packaging. A cracked bottle. A seal that didn’t hold. A label that got mixed up. One batch of pills labeled for high blood pressure might actually be a diabetes drug. That’s not a typo—that’s contamination of the most dangerous kind. And while the FDA tries to catch these before they reach you, the system isn’t perfect. Manufacturing happens all over the world, and oversight varies.
What can you do? Check your pills. Know your pharmacy. Keep your meds in their original containers. If your prescription suddenly looks different, ask. Don’t assume it’s just a new generic brand. And if you hear about a recall—don’t wait. Contact your doctor or pharmacist immediately. You don’t need to panic, but you do need to act.
Below, you’ll find real cases, expert breakdowns, and practical steps to avoid risky meds. From how a single contaminated batch can affect hundreds of transplant patients to why some states ban generic swaps for high-risk drugs—this collection gives you the facts you need to protect yourself and your family.
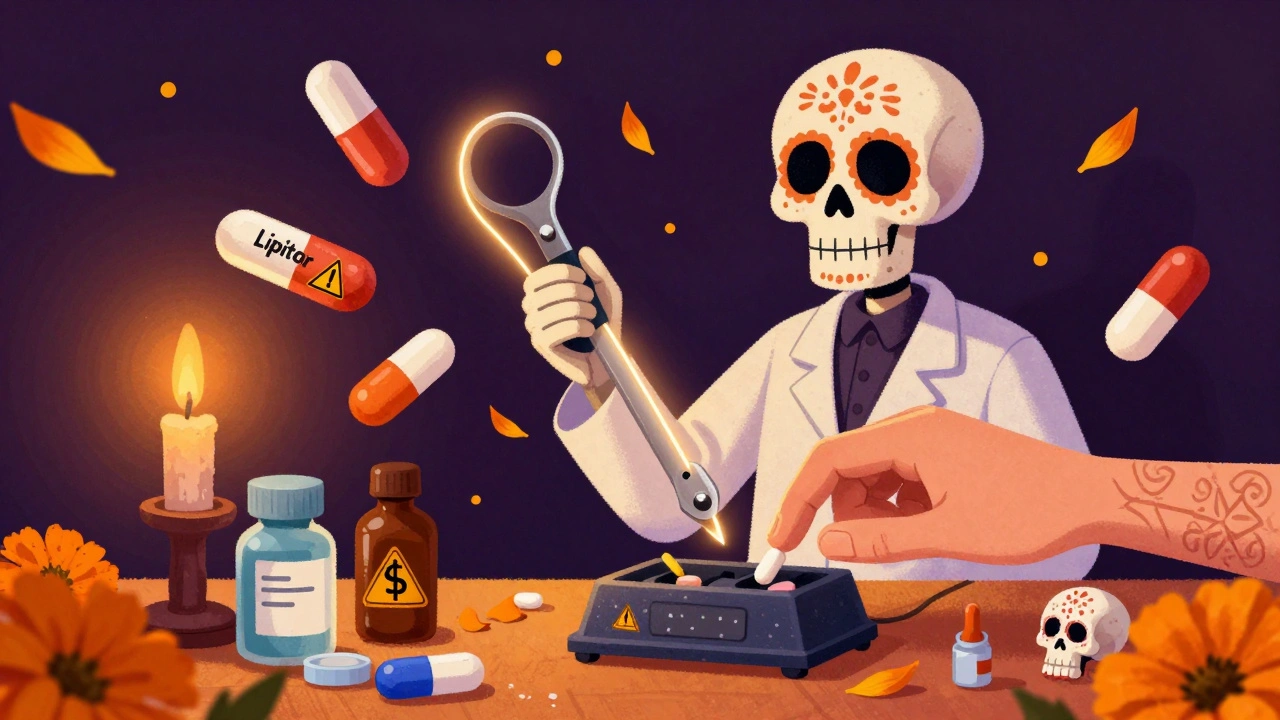
How to Avoid Contamination When Splitting or Crushing Pills: A Safe, Step-by-Step Guide
Learn how to safely split or crush pills without risking contamination, inaccurate dosing, or exposure to hazardous drugs. Follow proven steps, use the right tools, and know which pills should never be touched.