Patient Rights: How to Refuse Generic Substitution and Request Brand-Name Drugs
 Feb, 15 2026
Feb, 15 2026
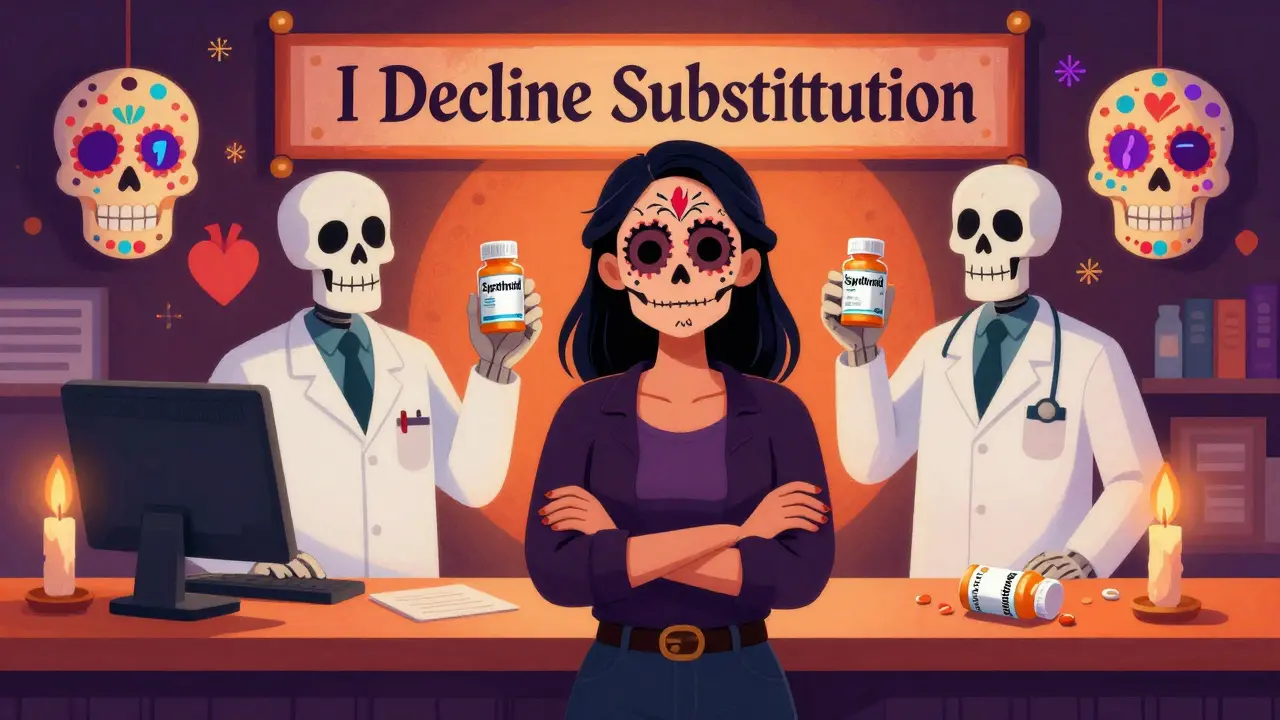
When you walk into a pharmacy to pick up your prescription, you might not realize you have the legal right to say no. Many patients assume the pharmacist will automatically swap their brand-name drug for a cheaper generic version - and that’s often true. But generic substitution isn’t mandatory everywhere. In fact, in many states, you can refuse it outright - and the pharmacy must honor your request.
What Is Generic Substitution?
Generic drugs contain the same active ingredients as brand-name drugs and are approved by the FDA as therapeutically equivalent. They’re cheaper because they don’t require the same costly research and marketing. On average, generics cost 80-85% less than their brand-name counterparts. That’s why pharmacies and insurers push them - and why they make up over 90% of all prescriptions filled in the U.S. But here’s the catch: not all drugs are created equal. For some conditions - like epilepsy, thyroid disease, or diabetes - even tiny differences in how a drug is absorbed can cause serious problems. That’s why patients need to know their rights.Your Legal Right to Refuse
In 19 states, pharmacists are required to substitute generics automatically - no questions asked. But in 7 states plus Washington, D.C., the law says: you must consent first. That means if you say, "I don’t want the generic," the pharmacist can’t give it to you - even if it’s cheaper. These states are: Alaska, Connecticut, Hawaii, Maine, Massachusetts, New Hampshire, Vermont, and Washington, D.C. In these places, the pharmacy must get your permission before switching your medication. You don’t need to explain why. Just say: "I decline substitution." That’s legally binding. Even in states where substitution is automatic, you still have rights. Thirty-one states and D.C. require pharmacists to notify you - in writing or verbally - before making the switch. If they don’t tell you, you can refuse the drug and ask for the brand-name version instead.When Brand-Name Drugs Are Necessary
Some medications have a narrow therapeutic index (NTI). That means the difference between a dose that works and one that’s dangerous is very small. Examples include:- Levothyroxine (for thyroid conditions)
- Warfarin (a blood thinner)
- Phenytoin and carbamazepine (for seizures)
- Insulin (especially long-acting types like Lantus)
What to Say at the Pharmacy
You don’t need a degree in law to protect yourself. Here’s what works:- When the pharmacist says, "I have a generic version," reply: "I decline substitution. I want the brand-name drug as prescribed."
- If they argue, ask: "Can I speak to the manager?"
- If they say, "We have to substitute," respond: "I’m aware of my rights under state law. I’m not accepting the generic."
- If they still refuse, ask for a copy of your state’s pharmacy substitution law. Most pharmacies keep a printed copy on file.

What Doesn’t Work
Don’t say: "I can’t afford the brand-name." That opens the door for them to push you toward the generic - even if you don’t want it. Don’t assume your insurance will cover the brand. In many cases, it will - especially if your doctor has written "brand medically necessary." Some plans even cover brand-name drugs at no extra cost if there’s a medical reason. Don’t let pharmacists pressure you with phrases like "It’s the same thing." It’s not. Different inactive ingredients - like fillers, dyes, or coatings - can affect how your body absorbs the drug. That’s why some patients react badly after a switch.What to Do If You’re Switched Without Consent
If you were given a generic drug without your permission - especially for an NTI medication - take action:- Keep the prescription label and the new pill bottle.
- Call your doctor and report the switch.
- File a complaint with your state’s Board of Pharmacy. All 50 states have a process for this.
- If you had a bad reaction - like seizures, irregular heartbeat, or extreme fatigue - report it to the FDA’s MedWatch system.
How to Protect Yourself Long-Term
- Keep a list of all medications where you refuse substitution. Note the drug name, the reason, and the date. - Ask your doctor to add "dispense as written" to future prescriptions - even if you’re not currently having issues. - Use the FDA’s Orange Book (online) to check if your drug has an AB rating (substitutable) or an AB/other rating (may not be). You don’t need to be an expert - just know your drug’s rating. - Call ahead to your pharmacy before picking up. Ask: "Will you be substituting my medication?" If they say yes, say: "I decline. I need the brand-name." - Know your state’s law. A quick Google search - "[your state] pharmacy generic substitution law" - will pull up the exact rules.Why This Matters
Generic substitution saves the system billions. But at what cost? The Congressional Budget Office estimates that non-medical switching - changing stable patients to generics without medical need - costs the healthcare system $2.1 billion a year due to extra doctor visits, ER trips, and hospitalizations. You’re not just saving money. You’re protecting your health. If a drug works for you, don’t let someone else decide to change it - especially if you’re on a medication where small differences matter.FAQ
Can a pharmacist refuse to give me my brand-name drug if I ask for it?
No, not if you’re in a state that requires consent or if your doctor has written "dispense as written." In states like Massachusetts, Hawaii, and Vermont, pharmacists must honor your refusal. Even in states where substitution is automatic, you can still request the brand-name version - and if your doctor supports it, the pharmacy is legally required to fill it.
Will my insurance pay for the brand-name drug if I refuse the generic?
Often, yes - especially if your doctor notes "brand medically necessary." Many insurance plans cover brand-name drugs at the same cost as generics when there’s a medical reason. Even if your plan normally requires a higher copay, the pharmacy can sometimes apply a patient assistance program or coupon to bring the price down. Always ask: "What’s my out-of-pocket cost for the brand?"
Can I get my brand-name drug even if it costs more than the generic?
Yes. The law doesn’t require you to choose the cheapest option. Your health comes first. If you’ve been stable on a brand-name drug for months or years, you have the right to stay on it - even if the generic is cheaper. Pharmacists can’t pressure you into switching just because of cost.
What if the pharmacist says they "have to" substitute?
That’s false. In 19 states, pharmacists are required to substitute - but even there, you can still refuse. In the other 31 states, they must notify you first. In 7 states plus D.C., they need your consent. If they claim they "have to" substitute, ask to speak to the manager. Most pharmacists aren’t trained on state laws - but managers usually are.
Are biosimilars treated the same as generics?
No. Biosimilars - like those used for diabetes or rheumatoid arthritis - are not considered interchangeable like small-molecule generics. Forty-seven states now require explicit patient consent before switching to a biosimilar. Always ask: "Is this a biosimilar?" If yes, you have stronger rights to refuse.
Philip Blankenship
February 16, 2026 AT 23:29Man, I’ve been on levothyroxine for 12 years and switched generics twice - both times I felt like I was dragging a concrete blanket around. First time, I thought it was stress. Second time, I was dozing off at my desk at 2 p.m. like a zombie. Then I remembered this post’s advice - said "I decline substitution," and got my Synthroid back. No more naps. No more panic. Just me, my coffee, and my thyroid working right. Pharmacies act like they’re doing you a favor, but really, they’re just trying to hit their quota. You’re not the problem - the system is.
John Haberstroh
February 17, 2026 AT 07:32It’s wild how the FDA calls generics "therapeutically equivalent" but the real world says otherwise. I work in biotech, and even we can’t replicate the exact crystalline structure of some drugs - let alone the fillers and binders. One guy I know went from brand-name carbamazepine to generic and started having micro-seizures while driving. He didn’t even know it was happening until his wife noticed he’d stop blinking mid-conversation. That’s not equivalence - that’s Russian roulette with your brain. And yeah, the system saves pennies, but someone’s paying in neurological damage.
Carrie Schluckbier
February 18, 2026 AT 13:21Of course they push generics. Big Pharma owns the pharmacies, the insurers, the FDA, and half the state legislatures. You think this is about cost? Nah. It’s about control. They want you dependent on their supply chain. The moment you start asking for brand-name, you’re a threat. That’s why they’ll lie, gaslight you, and pretend they "have to" substitute. They’re scared you’ll figure out the whole thing’s a scam. Wake up. This isn’t healthcare - it’s a corporate prison.
Adam Short
February 19, 2026 AT 11:28This is why Britain’s NHS is better - no one’s playing pharmacy roulette. We get what the doctor prescribes, period. No "consent" nonsense. No "switching." No "you can ask" - because asking shouldn’t be necessary. You’re not a customer. You’re a patient. And if you’re on a drug that’s been stable for years, you don’t get to be experimented on just because someone’s profit margin needs a 30-cent boost. This isn’t freedom - it’s corporate feudalism with a pharmacy counter.
Liam Earney
February 21, 2026 AT 09:09...I just... I don’t know... I mean, I’ve been on warfarin for 15 years, and when they switched me last year... I didn’t realize it until my INR spiked to 6.8... I almost died... I had to go to the ER... and they said "it was just a generic"... and I thought... I thought I was being dramatic... but I wasn’t... I was just... trying to survive... and now I have a letter from my doctor taped to my fridge... and I call the pharmacy every time... and I still cry sometimes... because I’m so tired of fighting for my own body...
guy greenfeld
February 21, 2026 AT 09:45Here’s the real question: if a drug is so interchangeable, why does the FDA require a 10% bioequivalence window? Why not 1%? Why not 0.1%? Because they know - deep down - that biology isn’t math. That a pill isn’t a widget. That a human isn’t a data point. We’re not machines. We’re not supply chains. We’re fragile, evolving, biochemically idiosyncratic beings. And yet we’re treated like we’re running on Android updates. "Just reboot. It’ll be fine." No. No, it won’t be fine. And that’s not negligence - it’s a philosophical failure of modern medicine.
Sam Pearlman
February 21, 2026 AT 16:30Wait, so you’re telling me I can just say "I decline substitution" and get my Lantus without a fight? I’ve been paying $400 a month for this stuff. My insurance says "nope, generic only." But if I say no, they have to give me the brand? That’s wild. I’m gonna try it tomorrow. If it works, I’m telling everyone. If they kick me out, I’m starting a subreddit called r/PharmacyRebels. We’ll wear capes. And carry copies of state laws. I’m in.
Steph Carr
February 23, 2026 AT 00:52So let me get this straight - you’re saying that in 7 states and DC, you have to give consent before they swap your meds? That’s adorable. Like, "Oh, here’s your thyroid pill, ma’am, would you like the $2 version or the $120 one?" Meanwhile, in Texas, they’ll swap your insulin without telling you, then charge you $150 for a refill if you complain. So we’re not protecting patients - we’re running a patchwork quilt of healthcare apartheid. Some of us get dignity. Others get a pamphlet and a prayer.
Prateek Nalwaya
February 24, 2026 AT 21:34As someone from India where generics are the norm and brand-name drugs are luxury items, I’m stunned by how much resistance there is here. In Mumbai, we take generics because we have to - and most people are fine. But I’ve also seen patients suffer from inconsistent absorption. The difference here is that you have the legal framework to push back. That’s powerful. Maybe the real win isn’t just getting your brand-name drug - it’s realizing you have agency. That’s rare. That’s revolutionary. Keep asking. Keep refusing. It matters.
Jonathan Ruth
February 25, 2026 AT 15:49Generic substitution is a scam and everyone knows it. Pharmacies dont care about you they care about their cut from the manufacturer. My doc wrote dispense as written and they still tried to switch me. I called the state board they said oh weve had 17 complaints this month. So yeah. You think this is about safety? Its about profit. And if you dont fight its gonna keep happening. I printed the law and taped it to my prescription bottle. Now they see it and shut up. You want your life? You gotta take it.